Mpox
Updated: May 23, 2023
Mpox Surveillance Data - Inyo County
Inyo County Public Health will continue working with the California Department of Public Health and other local healthcare providers to monitor for Mpox, to provide health education, and to help control the spread of the virus. As of May 23, 2023, there have been zero (0) cases of Mpox virus reported among Inyo County residents.
To learn more cases in California: visit the California Department of Public Health's Mpox website provides information on the number of cases of mpox in California by County, as well as limited information on demographic groups affected by the virus. Information about cases by state can be found on the CDC's Monkeypox Situational Summary website. Since California’s first case of Mpox in May of 2022, the number of new cases was successfully reduced by working with federal, state, and local partners to distribute treatment and vaccines as well as boost awareness about the virus, which had been rarely seen before last year.
-----------------------------------------------------------------------------
Mpox Information, Symptoms,
About Mpox
Mpox is a rare disease that is caused by infection with the mpox virus. The mpox virus belongs to the Orthopoxvirus genus, which includes the variola (smallpox) virus as well as the vaccinia virus, which is used in the smallpox vaccine. Mpox is a public health concern because it can be transmitted person-to-person and can cause severe disease in humans. Although mpox virus is in the same family of viruses as smallpox, it is less transmissible and typically less severe than smallpox.
Mpox was first identified in 1958 and primarily occurs in Central and West African countries. Historically, mpox has been rare in the U.S. and has mostly been related to international travel or the importation of animals. In 2022, there has been a significant increase in reported cases in locations where mpox is not commonly seen, including Europe, Canada, and the United States, including California.
Symptoms
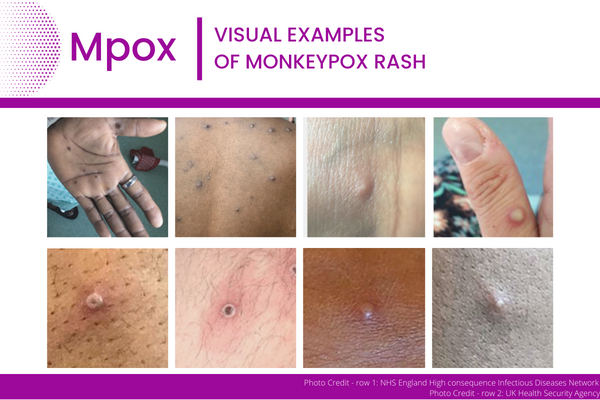
Mpox often starts with symptoms like the flu, with fever, low energy, swollen lymph nodes, and general body aches. Within 1 to 3 days (sometimes longer) after the appearance of fever, most infected people develop a rash or sores. The sores go through several stages, including scabs, before healing. The sores can look like pimples or blisters and may be painful and itchy.
The rash or sores may be located on or near the genitals (penis, testicles, labia, and vagina) or anus (butt) but can also appear on other areas like the hands, feet, chest, face, or inside the mouth. They may also be limited to one part of the body.
People with mpox may experience all or only a few of these symptoms. Most people with mpox will develop the rash or sores. Some people have reported developing a rash or sores before (or without) the flu-like symptoms.
Infectious Period
Mpox can spread from the time symptoms start until all sores have healed, scabs are off and a fresh layer of skin has formed underneath. This can take several weeks.
Transmission
Mpox can be spread by:
- Direct skin-to-skin contact with the sores or scabs of people with mpox
- Direct contact with body fluids of people with mpox, such as drainage from skin sores or saliva that was in contact with mouth sores
- Contact with the respiratory secretions of people with mpox, such as saliva, during prolonged, face-to-face contact or during intimate physical contact, such as kissing, cuddling, or sex
- Touching items (such as bedding, towels, clothing, cups and utensils) that previously touched the sores or body fluids of people with mpox
To date, there has been no evidence that mpox is spread by:
- Attending an outdoor event with fully clothed people
- Trying on clothes or shoes at a store
- Traveling in an airport, on a plane or on other public transit
- Swimming in a pool or body of water
- Casual contact with other people
If you believe you may have exposed someone to mpox while you were infectious, you can let them know anonymously, so that they can get tested as soon as possible. Please visit the CDPH Sexually Transmitted Disease (STD) website and refer under Quick links. Testing is strongly encouraged to help identify and prevent infections.
If you have been exposed to mpox, monitoring symptoms and avoiding sexual contact with others for 21 days is highly recommended. Mpox vaccination is most effective when obtained as soon as possible after exposure and is strongly encouraged for high-risk patients to prevent severe illness. For more information visit CDPH Mpox Vaccine Q&A.
Prevention
There are number of ways to prevent the spread of mpox, including:
- Always talking to your sexual partner/s about any recent illness and being aware of new or unexplained sores or rashes on your body or your partner's body, including on the genitals and anus
- Avoiding close contact, including hugging, kissing, cuddling and sexual activity with people who have symptoms like sores or rashes
- Not sharing materials (bedding, towels, clothing, utensils, cups) with someone who has symptoms
- Washing your hands often with soap and water or an alcohol-based hand sanitizer
- Using appropriate personal protective equipment (PPE) like a mask, gown, and gloves when caring for others with symptoms
- Avoiding contact with infected animals
Testing & Isolation
If you have a new or an unexplained rash or other symptoms, seek medical care for further testing and evaluation.
- Wear a well-fitting mask, ensure your rash is covered, and tell your health care provider that you have possible mpox symptoms.
- If you do not have a health care provider or healthcare insurance, visit a public health clinic or local county clinic. You may also contact the Department of Healthcare Services for more available resources.
- Avoid crowds and close contact, including sexual or intimate contact, until you see your health care provider.
For more information about isolation recommendations, please refer to the CDPH Mpox Home Isolation Guidance for the General Public.
Treatment
Most mpox infections are mild and will heal without any treatment. However, antiviral drugs, such as tecovirimat (TPOXX), may be used to treat mpox. This drug may be recommended for people who are more likely to get severely ill or for people who are experiencing severe disease. It may also be recommended for people who have rash or sores in areas that may be at higher risk for severe complications, such as the eyes or the genital area.
People who may be at risk for more severe illness include those with a weakened immune system, young children (less than 8 years of age), those who are pregnant or breastfeeding, and those with a history of certain skin diseases like eczema.
For more information on treatment, please visit the CDC Patient's Guide for Tecovirimat and the CDPH Mpox Tecovirimat Treatment Information for Providers guidance.
Tecovirimat should be administered early in the course of illness along with supportive care and pain control relief for those that are high risk for progression to severe disease.
It is important to talk to your health care provider if you have symptoms of mpox and are experiencing pain or irritation due to the rash or sores. Your provider may also be able to offer treatments that are not specific to mpox, but may help to reduce your symptoms, like prescribed mouth rinses, stool softeners for those with rectal pain, or topical gels or creams.
Vaccination
Vaccination helps protect against mpox when given before or shortly after an exposure and is highly recommended for high-risk patients. See the CDPH mpox vaccine page to learn more about the JYNNEOS vaccine and where to get vaccinated.
Additional Information
For more information about mpox, visit the CDPH Mpox Q&A.